This post is a CALL TO ACTION to fight COVID-19!
Grandparents and Parents, please use your voices!
Help us tell health care workers about the research-based
methods to disinfect personal protective equipment.
Researchers have developed three protocols to disinfect N95 masks
2. Stanford Medical Center has determined two protocols for sanitizing N95 masks: hot air and UV
What do we asking grandparents and parents to do?
Please, Grandparents and Parents, use your voices! Pass along this article to EVERY person ─ husband, wife, son, daughter, niece, nephew, friend, neighbor, etc. ─ you know who works in any aspect of healthcare, including emergency services. Ask them to forward this information to the administrators of their hospitals and to the heads of the institutions and entities for whom they work.
The information in this post is technical, but it can save lives… with your help!
Why is this information important?
There is a critical shortage of N95 masks, and your action could save lives. We have found not every medical entity, doctor, nurse, first responder, medical professional, and staff person knows how to sanitize N95 masks effectively to extend their usefulness with methods that ensure no physical or performance degradation. The information we are asking you to pass along has been developed by highly regarded medical institutions: the University of Nebraska Medical Center, Stanford University Medical Center, and Duke University and Health Center. Our trying to get through to the decision makers is difficult because they are juggling so much in the midst of this pandemic. Your personal connection to a medical professional makes the odds of the research about these decontamination methods getting to the right person an almost sure thing. PLEASE! Pass along this information now!
Are these methods expensive?
No. N95 mask decontamination is inexpensive, easy to implement, and easy to accomplish; there is no reason for healthcare professionals and first responders not to be protected even in the face of this significant global shortage of personal protective equipment (PPE). The information we have gathered allows for repeated decontamination of the N95 masks and extends the use of each for as long as two weeks. It is imperative that medical professionals and first responders have access to these protocols now.
Effective decontamination extends the life of a mask from one use or one day to use multiple days or even weeks and significantly reduces exposures to the virus. This is important for patient safety as well as for the health of medical professionals ─ many of whom have contracted COVID-19, and, sadly, many of whom have died. NOW is the time to get this information into the hands of medical decision makers!
Is reusing N95 masks against the recommendation of the National Institute for Occupational Safety and Health (NIOSH)?
Yes, it is. However, there is a severe global shortage of PPE. We have gathered information from websites and posted it here for the sole purpose of saving lives. DISCLAIMER: We are not medical professionals, but we have friends and relatives who are, and we want to help keep them safe! Each person and entity who chooses to use this information should seek approval from his or her own administration before implementing any of these methods. We hope that upon seeking approval, the administrators will adopt these methods system wide.
What are the protocols?
This is the technical information hospital administrators
will need to decide which decontamination method to implement:
The University of Nebraska Medical Center uses
big ultraviolet (UV) light towers to decontaminate the N95 masks,
making them reusable for up to two weeks
https://www.nebraskamed.com/COVID/how-were-using-ultraviolet-light-to-slow-the-n95-mask-shortage
“After each use, health care workers put their masks in a paper bag.
“The bag then goes to a room equipped with a UV light tower. The big tower, which gives off an eerie blue glow when turned on, normally lives in the Nebraska Biocontainment Unit. It’s used to decontaminate rooms after patients leave. The ultraviolet light disrupts the coronavirus’s genetic material, deactivating it.
“In the new decontamination room, masks hang across long, thin wires, resembling a clothesline. Then the UV tower goes to work. Once it’s finished, the masks are removed, re-bagged, and returned to their original owners for reuse.”
Ultraviolet Decontamination of N95 Filtering Facepiece Respirators
https://www.nebraskamed.com/sites/default/files/documents/covid-19/n-95-decon-process.pdf
The evidence base supporting this program includes: 1) Ultraviolet germicidal irradiation (UVGI) “has been shown to effectively inactivate a wide range of human pathogens including coronaviruses and other human respiratory viruses; 2) UVGI has been demonstrated to inactivate human respiratory viruses, including coronaviruses, on various models of N95 respirators; 3) levels of UVGI needed to inactive human respiratory viruses are well below the level of irradiation that adversely affects the fit and filtration characteristics of N95 FFRs; and 4) UVGI can be safely administered when appropriate safeguards are in place. Herein, we briefly describe our procedure to decontaminate and reuse N95 respirators.
“Used N95 FFRs are subjected to UV-C at an exposure of 60 mJ/cm2. Single-stranded RNA viruses, such as SARS-CoV-2, are generally inactivated by UV-C exposure of 2-5 mJ/cm2 (1). Thus, the UV-C exposure we have chosen exceeds, by at least several fold, the amount of exposure needed to inactivate SARS CoV-2 and provides a wide margin of safety. Respirators are secured on wires that are strung across a room with two UV towers (ClorDiSys UV-C Light System, https://www.clordisys.com/products.php) on either side. Our UV-C towers are equipped with eight 254 nm bulbs that are routinely used in biosafety cabinets and produce 200 μw/cm2 at 10 feet distance for a dosage of 12 mJ/minute. We monitor the delivered UV exposure dose with a UV meter that can be initiated and monitored from outside the room to verify that the desired exposure has been achieved. We plan to decontaminate and reuse the N95 respirators multiple times until respirator fit is impacted (2-4). Prior to initiating the decontamination program, the walls and ceiling were covered with a UV-reflective coating (https://lumacept.com) with which our group had experience (5) Our program initially involved the units with high N95 respirator use such as the emergency department and our COVID19 ward, but we plan to rapidly expand to ambulatory settings. We believe a variety of UV light source could be used in a similar fashion including UV equipped biosafety or sterilization cabinets or other UV disinfection systems and that this method can be applied to a variety of other critical items such as procedure masks.”
Stanford Medical Center has determined
two protocols for sanitizing N95 masks
https://stanfordmedicine.app.box.com/v/covid19-PPE-1-2
Stanford researchers determined two disinfection methods of N95 masks do not reduce the filtration efficiency of the meltblown layer after an appreciable number of treatment cycles. The researchers found: Method 1, 75 °C Hot air (30 min) for 20 cycles; Method 2, UV (254nm, 8W,30 min) for 10 cycles.
Stanford warns: Do not use anything in your
home to disinfect contaminated equipment.
Please do not heat your masks in a home oven or microwave!
Duke University and Health Center utilizes
Hydrogen 31 Peroxide Vapor to decontaminate
and reuse N95 respirators for up to 30 times
https://www.safety.duke.edu/sites/default/files/N-95_VHP-Decon-Re-Use.pdf
“Duke University houses one of the National Institute of Allergy and Infectious Diseases (NIAID) Regional Biocontainment Laboratories (RBL).” The staff collected “approximately 100 [N95 masks], previously used in quantitative employee fit testing,… and [hung them] from stainless steel wire racks in [its] Hydrogen Peroxide Vapor processing room in the RBL, the Hydrogen Peroxide Vapor run consisted of the following five stages: Conditioning, Pre-gassing, Gassing, Gassing Dwell and Aeration. The existing RBL Hydrogen Vapor standard operating procedure (SOP) was employed and requires that the processing room attain 480+ ppm level of Hydrogen Peroxide Vapor with a “Gassing” time of 25 minutes and a “Gassing Dwell” time of 20 minutes. At the end of a cycle, during the aeration stage, fresh air is introduced into the room to increase the rate of catalytic conversion of hydrogen peroxide vapor into oxygen and water. This procedure leaves no residue other than water. When sufficient time had passed, [staff] used a PortaSensII™ sensor to ensure hydrogen peroxide levels are below the OSHA Permissible Exposure Limit3 (PEL) of 1.0 ppm prior to entering the room. In addition, [staff] validated the efficacy of the decontamination process by using eight individual 6-log biological indicators the efficacy of the decontamination process by using eight individual 6-log biological indicators (Geobacillus stearothermophilus spores.)”
Conclusion: “Using Hydrogen Peroxide Vapor
is a proven method of decontamination.”
According to a cnn.com article, the Duke University team can clean as many as 500 masks at a time. The process takes more than four hours.
Strategies for Optimizing the Supply of N95 Respirators
https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html
From the CDC website: The following strategies are based upon these assumptions: 1) facilities understand their current N95 respirator inventory and supply chain, 2) facilities understand their N95 respirators utilization rate, and 3) facilities are in communication with state and local public health partners (e.g., public health emergency preparedness and response staff) and healthcare coalitions. While these strategies are targeted for optimizing the supply of N95 respirators, some of these strategies may be applicable to optimizing the supply of other personal protective equipment such as gowns, gloves, and eye protection.
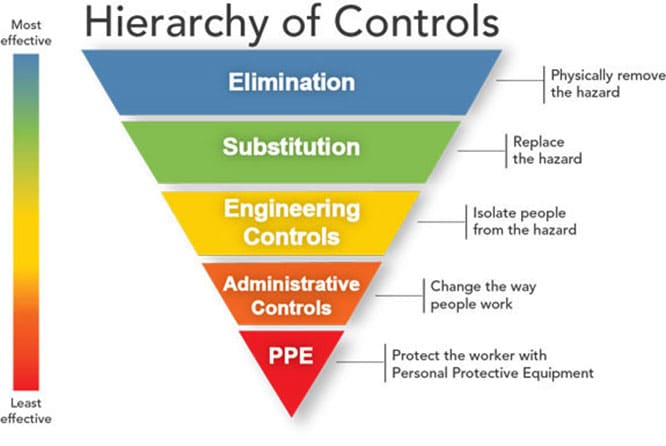
Controlling exposures to occupational hazards is a fundamental way to protect personnel. Conventionally, a hierarchy has been used to achieve feasible and effective controls. Multiple control strategies can be implemented concurrently and or sequentially. This hierarchy can be represented as follows:
- Elimination
- Substitution
- Engineering controls
- Administrative controls
- Personal protective equipment (PPE)
To prevent infectious disease transmission, elimination (physically removing the hazard) and substitution (replacing the hazard) are not typically options for the healthcare setting. However, exposures to transmissible respiratory pathogens in healthcare facilities can often be reduced or possibly avoided through engineering and administrative controls and PPE. Prompt detection and effective triage and isolation of potentially infectious patients are essential to prevent unnecessary exposures among patients, healthcare personnel (HCP), and visitors at the facility.
N95 respirators are the PPE most often used to control exposures to infections transmitted via the airborne route, though their effectiveness is highly dependent upon proper fit and use. The optimal way to prevent airborne transmission is to use a combination of interventions from across the hierarchy of controls, not just PPE alone. Applying a combination of controls can provide an additional degree of protection, even if one intervention fails or is not available.
Respirators, when required to protect HCP from airborne contaminants such as infectious agents, must be used in the context of a comprehensive, written respiratory protection program that meets the requirements of OSHA’s Respiratory Protection standard. The program should include medical evaluations, training, and fit testing.external he program should include medical evaluations, training, and fit testing.
The Ohio company says its process could decontaminate 80,000
masks per day using a “vapor phase hydrogen peroxide” process.
Simply copy the link in the address bar and send it to all the medical personnel you know! Thank you!
Dana M. Conklin has a special interest in ensuring hospitals are sanitizing N95 masks following protocols that ensure the least damage to each mask. She is a fiduciary in Northern California, and her clients primarily are senior citizens, who are at high risk for contracting COVID-19. Conklin spent five months in China, including Wuhan. As she watched the nightmare unfold in China earlier this year, she remembered the national shortage of N95 masks during the recent California wildfires. She then read an article in the New York Times about an innovative method the University of Nebraska Medical Center is using to decontaminate N95 masks. Her friends who work at large metropolitan area hospitals knew of no credible method for cleaning their masks. One longtime friend, a nurse at a hospital in one of Florida’s current hot spots, told her an emergency department nurse had been handed a bandanna upon arriving at work the morning before. Horrified, Conklin began collecting credible N95 decontamination information and sharing it via calls to hospitals and first responders and via the Internet. You can reach Conklin at danamail@earthlink.net.
Carolyn Berry has a special interest in helping medical professionals stay safe because her younger son is a doctor in Virginia Beach, VA. She has friends who are nurses and friends who are parents of nurses and other healthcare professionals. She is the former public relations association for Virginia Beach General Hospital, then part of Tidewater Health Care, now Sentara Healthcare. She currently is writing a book for grandparents and their grandchildren. To sign up for her monthly newsletter, visit adventureswithgrammy.com/newsletter. You can reach her at carolyn@adventureswithgrammy.com.
###